Sep 22, 2023


By Stephanie Simons,
Head Pharmacist,
Lindo’s Pharmacy in Devonshire
September can mean many things. Back to school. The start of fall. You might even see a festive advert or two! But September is also Urology Awareness Month. While perhaps less exciting, it’s a highly important time, especially because of the stigma that surrounds urological conditions.
Urology covers a wide range of conditions, across urological cancers, diseases, and infections. The discomfort or awkwardness many of us feel when discussing them can mean people don’t know what their symptoms mean or how to support a child or other family member who is struggling. However, it’s vital for our health that we understand these conditions and the impact they can have on our and others’ lives.
This year, Urology Awareness Month is focused on bladder health, specifically urinary tract infections (UTIs), urinary incontinence, and bladder cancer.
UTIs and incontinence
Both UTIs and urinary incontinence are more likely to affect women. Two-thirds of women and approximately 12% of men will have at least one UTI at some stage of their life, whilst urinary incontinence affects 13% of women and 5% of all men.
A UTI occurs when bacteria get into your urinary tract, bladder, or urethra, causing the lining to become red and irritated. This can cause burning pain when urinating, and/or the strong urge to urinate even when your bladder isn’t full. You may also experience lower abdomen or back pain. To lower your risk, ensure you drink plenty of fluids to stay hydrated and don’t put off urinating when you need to.
 You can ease the symptoms by using products containing sodium citrate or potassium citrate such as Cymalon or Care Cystitis Relief which reduce the acidity of your urine to help prevent burning or irritating sensations. Phenazopyridine can also help to reduce pain and the sense of urgency to urinate. You may also need antibiotics to combat the infection; speak to your pharmacist or GP for advice.
You can ease the symptoms by using products containing sodium citrate or potassium citrate such as Cymalon or Care Cystitis Relief which reduce the acidity of your urine to help prevent burning or irritating sensations. Phenazopyridine can also help to reduce pain and the sense of urgency to urinate. You may also need antibiotics to combat the infection; speak to your pharmacist or GP for advice.
Like UTIs, incontinence impacts more women as they get older, due to lowering oestrogen levels. Childbirth, both caesarean and vaginal, also heighten risk, increasing with each additional baby. Older men, meanwhile, are also at higher risk of incontinence, especially those experiencing prostate issues. For both men and women, poor overall health can lead to incontinence, such as diabetes, high blood pressure, and smoking.
Many people suffer in silence, but incontinence can be treated – and there’s no need to be embarrassed. Your pharmacist or GP can help advise on lifestyle changes like reducing alcohol or caffeine intake, losing weight, pelvic floor exercises, or bladder training which can all significantly help. You may also find products like Poise or Depend pads or undergarments and Femfresh or Summer’s Eve wipes and washes to improve your daily experience.
Bladder cancer
Bladder cancer is the sixth most common cancer in the United States, impacting around 84,000 people every year. It affects three times more men than women, and results in nearly 17,000 deaths annually.
Bladder cancer is when cancer cells are found in the tissue that lines the inner surface of the bladder. As with many cancers, the quicker you are diagnosed the higher your chance of recovery. Look out for key symptoms such as blood in the urine, pain in your lower abdomen, lower back and/or when you pass urine, as well as frequent and urgent urination. These symptoms don’t necessarily mean you have cancer, but you should always consult your doctor if and when they arise.
Your risk of bladder cancer increases with age. Take note if anything ever feels strange or unfamiliar and keep up your regular check-ups with your GP. Smokers are also at higher risk – if you need support quitting smoking, speak to your pharmacist for advice, guidance, and useful products such as Nicorette or Nicotinell.
How we can help
We know it can be difficult to discuss urological issues. However, health professionals are more than happy to provide a safe and supportive space to explore your fears or symptoms and advise on next steps. Just ask your pharmacist for a quiet place to chat or book an appointment with your GP. Awareness of these issues could save lives.
Stephanie Simons is the head pharmacist at Lindo’s Pharmacy in Devonshire. She earned her Bachelor of Science in Pharmacy at Massachusetts College of Pharmacy and has been practicing for over 20 years. She is a registered pharmacist with the Bermuda Pharmacy Council and is a member of the Bermuda Pharmaceutical Association.
Jul 24, 2023

By Stephanie Simons,
Head Pharmacist,
Lindo’s Pharmacy in Devonshire
Breakouts, scars, tan lines. We all have quibbles with our skin from time to time. Yet for some, their skin can cause long-term issues that impact their daily lives. Every August, Psoriasis Awareness Month aims to raise awareness of this significant condition so we can help support those who manage it throughout their lives.
What is psoriasis?
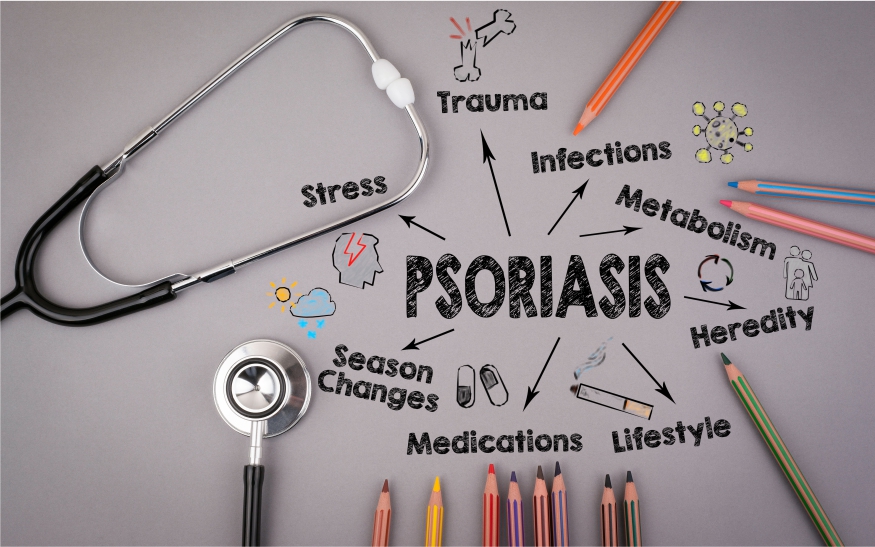
Psoriasis is a long-term condition that causes raised plaques on the skin that are often flaky, scaly, sore, and itchy. It begins in the immune system where immune cells (T cells) are triggered and act as if they were trying to heal the skin or fight infection. Inflammatory chemicals are produced, leading to overactive skin growth and an accumulation of skin cells, manifesting in itchy, raised plaques.
Plaques can occur on any area of the body but are most common on the scalp, hands, feet, and genitals. While some people suffer fairly constantly, others experience sporadic flare-ups that are triggered by a variety of factors, from stress or hormonal changes to infection or certain medications.
How is it treated?
There are a wide range of ways doctors treat this condition and it is often a process of trial and error.
Moisturising the skin can make it more comfortable by soothing the dryness, cracking, and itching. Many doctors recommend applying a moisturiser before using other topical treatments to help them absorb. Ingredients are key – avoid irritants such as artificial scents, and choose a texture that will suit your symptoms and lifestyle. For example, lotions like Cetaphil, Eucerin, and E45 absorb well in more hairy areas, lighter creams like Eucerin and Cerave can be more comfortable in the daytime, while oil-rich creams or ointments like Aquaphor, Emulsifying ointment or Aqueous Cream are better saved for before bed.
Your GP is also likely to prescribe topical treatments. Vitamin D is commonly used to slow the overactive production of skin cells, thus improving psoriasis symptoms. Vitamin D is often prescribed in combination with a topical steroid to reduce irritation, and/or coal tar oil which has anti-scaling properties. This type of treatment is generally prescribed to treat small areas of skin.
Where topical treatments are less effective, your doctor may recommend UV treatments. Applied by medical professionals in a phototherapy unit, narrowband UVB can treat larger areas where topical treatments are not suitable or have proven ineffective. PUVA combines UVA with psoralen which makes the skin more sensitive to the rays.
How to manage psoriasis
Your GP can help you develop a care plan that works for you. The psychological impact of psoriasis can be equally difficult and this should form a key part of your key plan. Remember not to stop using your treatments if your psoriasis clears up (unless recommended by your GP) as treatments also prevent further flare-ups from occurring.
While important for everyone, self-care is crucial for those managing long-term conditions. Eating a healthy diet rich in fruit and vegetables and limiting unhealthy choices like smoking or binge drinking will always reduce the likelihood of a flare-up. If your symptoms worsen when you’re stressed or anxious, set aside more time for relaxation – whatever that looks like for you. Your pharmacist will be happy to help build a self-care routine, with suggestions like Ashwagandha, Vitamin B-Complex, or Stress Away (or Goodbye) gummies to boost your mood and calm your mind.
If you’re suffering from psoriasis or have concerns about your skin, do speak to your GP or pharmacist.
Stephanie Simons is the head pharmacist at Lindo’s Pharmacy in Devonshire. She earned her Bachelor of Science in Pharmacy at Massachusetts College of Pharmacy and has been practicing for over 20 years. She is a registered pharmacist with the Bermuda Pharmacy Council and is a member of the Bermuda Pharmaceutical Association.
Jun 22, 2023

By Stephanie Simons,
Head Pharmacist,
Lindo’s Pharmacy in Devonshire
We all like a sweet treat sometimes, whether it’s a biscuit with our coffee, or an ice cream cone on the beach. And there’s never a better time to indulge your sweet tooth than June, for this month is National Candy Month!
From Hersey bars and M&Ms to gummy bears and Licorice Laces, we all have our favourites and there’s nothing wrong with a little indulgence every now and then. But if we eat too many of our favourite sweets, we can damage our bodies and heighten our risk of serious health conditions.
What is sugar?
Sugar is not a bad thing, in and of itself. All plants make sugar through photosynthesis, the process through which they turn sunlight into food. Sugar beets and sugar cane are most efficient plants from which to extract sugar as they make the greatest quantities. Glucose from sugar is used by the body as fuel and plays a key role in getting energy to your brain, organs and muscles.
Sugar in food
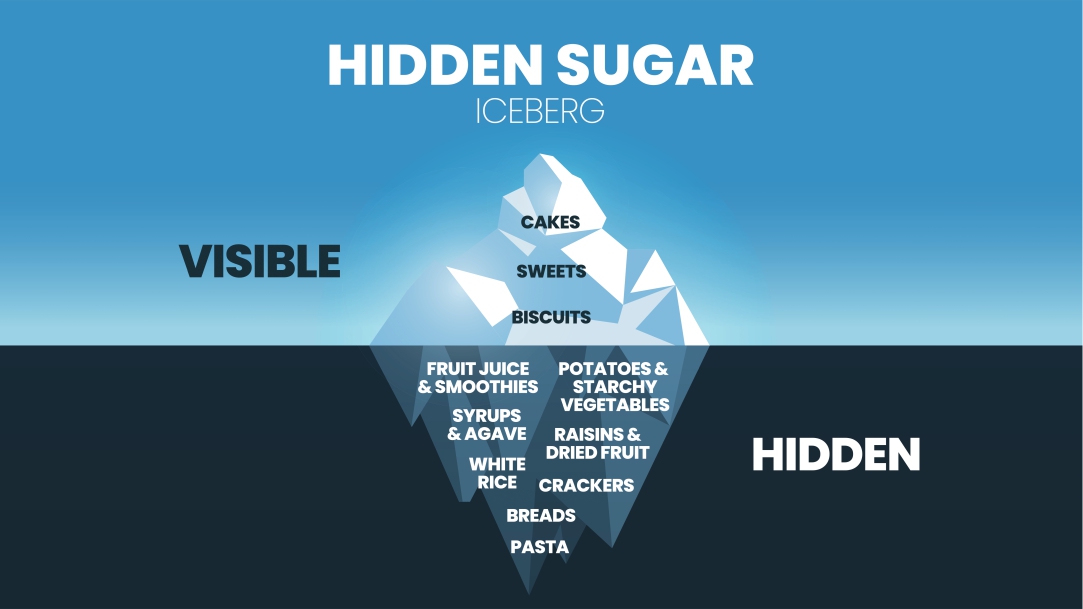
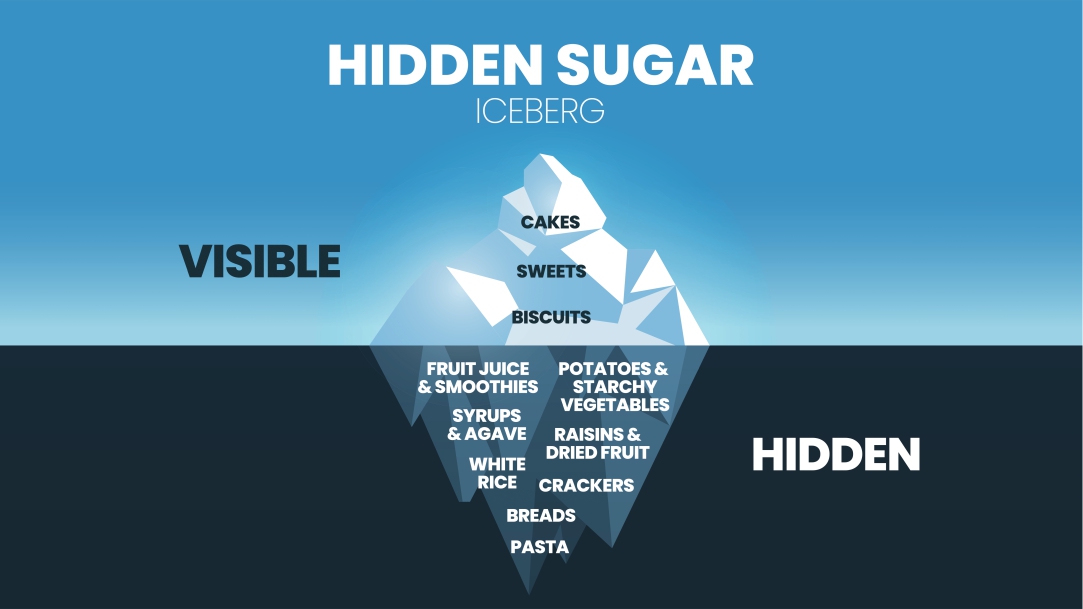
The problem comes when ‘free’ or ‘simple’ sugars are eaten in too large a quantity. Some foods like fruit and vegetables naturally contain sugar but within the structure of the food it is far less harmful. However, when sugar is added to foods and recipes (or indeed when fruits are juiced or pureed, thus losing their structure) the sugar is defined as ‘simple’ and can have a damaging impact on the body.
It’s surprisingly easy to eat too much sugar, even if you’re not a candy fan. Sugar is added to so much of the food we eat, sweet and savoury, for a multitude of reasons from balancing acidity to preventing spoilage. Often low-fat foods like yoghurt have added sugar to enhance the flavour, as do sauces like ketchup or barbecue sauce. Ready meals and pre-made soups often contain a lot of sugar too.
In the United States, it’s estimated that the average adult consumes 17 teaspoons of added sugar each day – deriving 14% of their total calories (4% higher than the recommended maximum 10%).
The trouble with sugar
So, what exactly is the problem with sugar?
For a start, a diet high in sugar is often lacking in the nutrients your body needs to function and feel its best. Foods that are high in added sugar are often also high in calories, while certain sugars trigger an increase in appetite and inhibit your body’s ability to realise it’s full. Ultimately, these issues can cause weight gain and potentially obesity.
Both high sugar intake and obesity dramatically increase your risk of Type 2 diabetes. Excess abdominal fat causes fat cells to release ‘pro-inflammatory’ chemicals that cause insulin resistance – the key characteristic of Type 2 diabetes. There is also evidence that high sugar diets can lead to inflammation, high triglycerides, blood sugar and blood pressure levels – all of which put you at high risk of heart disease.
Consuming vast quantities of sugar can also damage your skin. Sugary foods can cause blood sugar and insulin spikes and the resulting increase in androgen secretion, oil production, and inflammation can aggravate the skin and cause acne. Increased reactions between sugar and protein, furthermore, result in advanced glycation end products (AGEs) which can cause your skin to age prematurely.
Reducing your sugar intake
While a little sweet treat every now and then is perfectly fine, it’s good to keep things in moderation. Firstly, get to know your labels. Even products marketed as health products such as cereal bars can contain high levels of sugar – it’s always worth checking Options like Larabar, Kind bars or other brands using Stevia as the sweetener offer the health benefits without the sugar. Increase the protein in your diet with white fish, whole grains, nuts and tofu to help you stay full and less likely to binge on sugary treats. Cooking your own meals and snacks is also a good way to monitor how much sugar goes you’re your food.
If you’re concerned about your blood sugar levels, try products with cinnamon or ginseng such as N.B. Cinnamon or Ginseng. Vitamin D and magnesium supplements like Nature’s Bounty or Nature’s Truth supplements are also thought to help manage blood sugar, while probiotics like Culturelle, PB8 and Wellbiotics can also help. If you’re at all worried about your health or would like support improving your diet, your GP or local pharmacist will always be happy to help.
Stephanie Simons is the head pharmacist at Lindo’s Pharmacy in Devonshire. She earned her Bachelor of Science in Pharmacy at Massachusetts College of Pharmacy and has been practicing for over 20 years. She is a registered pharmacist with the Bermuda Pharmacy Council and is a member of the Bermuda Pharmaceutical Association.
May 23, 2023


By Stephanie Simons,
Head Pharmacist,
Lindo’s Pharmacy in Devonshire
The sun’s out and the guns are out too! But for some, summer brings more than sunshine and days at the beach. We’re entering prime allergy season, and many people find the summer months more irritating than relaxing. Runny noses, sore eyes, and itchy throats are just a few symptoms that tend to flare up, but there are ways to avoid allergens and to soothe your symptoms should they arise.
What is an allergy?
An allergy is when your body reacts badly to an external trigger that is harmless for most people, such as a type of food or the fur of a specific animal. These triggers are known as allergens and can cause a range of allergic reactions from a mild rash to life-threatening anaphylactic shock. A key reason allergic reactions rise at this time of year is because a great number of allergens are present outdoors – and in the summer as we tend to spend more time outside, or else let the outside in through open windows and doors.
Summer allergies
Many summer allergies are caused by pollen from the grass, which reaches peak levels in the hotter months – and spreads all the more when people mow their lawns. Plants and flowers also give off more pollen in the summer as they grow bigger. Ragweed is one of the most common summer allergens; even if there’s none growing nearby, it can travel for hundreds of miles on the wind.
A range of other allergens flourish during the summer too. Mould can spread in warm, damp areas like basements and bathrooms, releasing spores into the air that trigger reactions. Dust mites also thrive in humid conditions and when their residue enters the air it can cause sneezing and runny noses.
Insects in general are far more prevalent in the summer as they make the most of high pollen counts and long hours of sunshine. Fire ants, bees, wasps, yellow jackets and hornets can sting if you get in their way and while most people experience only minor stinging, itching and/swelling – to those with severe allergies, it can be life-threatening. If you find your throat or tongue swelling, or experience dizziness or nausea after a sting, seek emergency medical help right away. Those with a known insect allergy may be prescribed an epinephrine auto-injector device (EpiPen) which can slow severe reactions so that sufferers can access medical help in time.
Others suffer in the summer due to sensitivity to heat and/or the sun itself. Prolonged exposure to strong sunlight can cause prickly heat or a heat rash – small, raised spots, an itchy, prickly feeling and/or mild swelling. Polymorphic light eruption, an allergy to sunlight, often exhibits similar rash-like symptoms. This can last for up to two weeks, but usually heals on its own and without scarring.
Soothing the symptoms
Good news – there are ways you can avoid allergens and treat reactions when they do occur. For those with air-borne allergies, keeping your doors and windows closed and using an air conditioner and/or an air purifier can help you dodge nasties from the outdoors. Cleaning air filters, vents and surfaces inside the home can also aid this process and keeping the humidity in your house between 30 and 50 per cent can prevent dust and mould from thriving. Insect repellent products like Off or Cutter which contain DEET or Alba Bug Away which is DEET free can help deter insects like mosquitos and wasps away from the body, preventing stings and adverse reactions.
If you do suffer from summer allergies, oral antihistamines such as Loratadine or Fexofenadine which are non-drowsy or Piriton or Benadryl which can cause drowsiness can help keep your symptoms at bay. Decongestants like Otrivin or Afrin (nasal sprays) or Sudafed an oral medication are also useful in treating cold-like symptoms that arise. If you’re experiencing reactions on your skin, calamine lotion or skin-soothing creams like Aveeno or any After Sun lotion with aloe can calm rashes and stings. Stronger treatments are available on prescription too – just ask your GP.
If you are concerned about an allergy or need help managing your symptoms, do speak to your pharmacist or GP who can advise on the best treatment – so you can enjoy the summertime free of irritation.
Stephanie Simons is the head pharmacist at Lindo’s Pharmacy in Devonshire. She earned her Bachelor of Science in Pharmacy at Massachusetts College of Pharmacy and has been practicing for over 20 years. She is a registered pharmacist with the Bermuda Pharmacy Council and is a member of the Bermuda Pharmaceutical Association.
Apr 16, 2023


By Stephanie Simons,
Head Pharmacist,
Lindo’s Pharmacy in Devonshire
Welcome back, summer! Though we Bermudians are lucky to get sunshine throughout the year, we still look forward to the summer months and the glorious weather they bring. That said, as the days start to really heat up, it’s important to take care of ourselves in the sunshine – and look out for those for whom the hot weather can pose a serious health risk.
Heat exhaustion
Heat exhaustion is a common bodily response to losing significant amounts of water and salt, often due to excessive sweating. Spending too long in the hot sun can cause heat exhaustion in all of us, whatever our age or health – and the risk is heightened with strenuous exercise. If you’ve been too hot for too long, you’re likely to experience a headache, nausea, and dizziness. Some people may also experience cramps in the arms, legs, and stomach and an increased heart rate while others may feel weak, irritable, or highly thirsty.
Heat exhaustion isn’t a danger in most cases if addressed quickly. Someone showing signs of heat exhaustion should move to a cooler environment out of the sun, remove unnecessary clothing like hats or jackets and drink plenty of water. It’s best not to leave anyone alone in this situation – they may need help cooling down if they feel weak or disoriented.
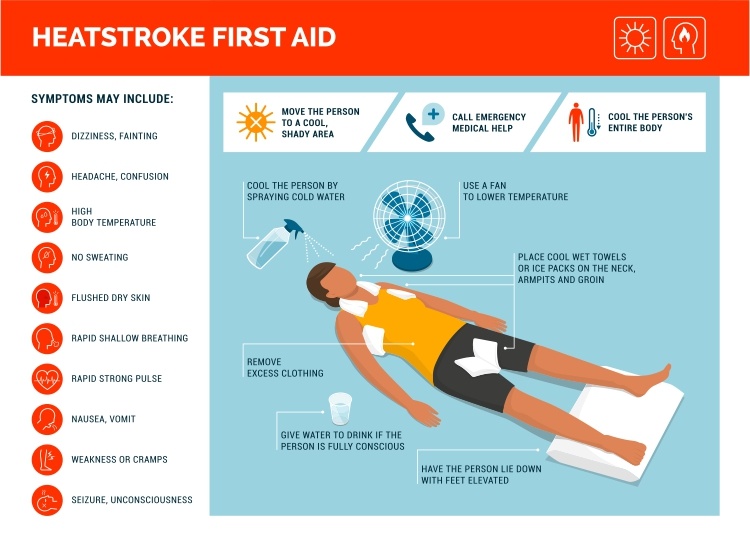
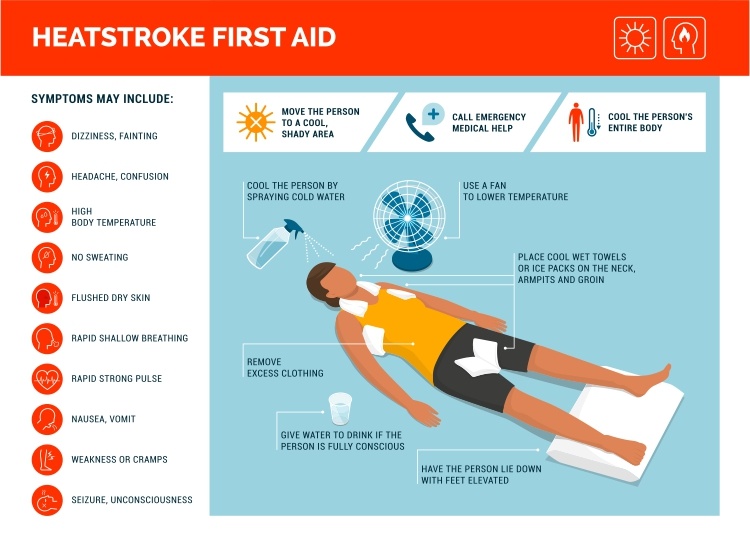
Heat stroke
Most people will cool down and feel better in about half an hour. If they don’t – this may indicate heat stroke, which can have much more serious consequences. If suffering from heat stroke, you will have a very high temperature, hot skin that isn’t sweating and/or a rapid heartbeat. Many will also experience confusion, lack of coordination, seizures, or even loss of consciousness. If you suspect heat stroke, it’s important to seek emergency healthcare as soon as possible.
 Who is vulnerable?
Who is vulnerable?
Extremely hot weather can be a serious health risk, particularly to those most vulnerable. It’s important to take care of those who may be most affected and ensure they are able to keep cool. Older people, generally those over 75, are at particular risk of heat stroke, especially if they live alone. Those with a long-term health condition such as heart or lung issues, Parkinson’s, diabetes, or certain mental health problems are also at greater risk. If you or someone close to you is at particular risk during the hot weather, keep an eye out to make sure they can stay cool and access the support they need during hot periods.
Staying cool in the heat
While we all enjoy a bit of fun in the sun, it’s important to limit your time in the heat – particularly between 11am and 3pm when the sun is strongest. When you are outdoors, stick to low-intensity activities like walking or relaxing and be sure to wear light, loose clothing. If you prefer to exercise outdoors, stick to early morning and late evening to avoid exertion in the heat. Choosing cold food and drinks while avoiding alcohol and caffeine can also help you stay hydrated.
If you do experience difficulties, your pharmacist can help. Rehydration sachets like Dioralyte or Pedialyte or tablets like Nuun, which are mixed into water and drunk can help you stay hydrated, and your pharmacist can also advise on sports drinks like Gatorade or Powerade which boost your natural hydration during hot weather. If your cheeks are feeling flush, we can help with skin care like Thayer’s Witch Hazel toners and Limacol to see you through the hot spell, as well as the best SPFs like Coppertone, Panama Jack, or Alba Botanica brands with an SPF of at least 30 which protects both face and body from the sun’s rays.
If you’re concerned about yourself, a friend, or a family member during the summer months, you can always contact your pharmacist or GP – or if you suspect sunstroke, call 911 immediately.
Stephanie Simons is the head pharmacist at Lindo’s Pharmacy in Devonshire. She earned her Bachelor of Science in Pharmacy at Massachusetts College of Pharmacy and has been practicing for over 20 years. She is a registered pharmacist with the Bermuda Pharmacy Council and is a member of the Bermuda Pharmaceutical Association.
Mar 20, 2023

By Stephanie Simons,
Head Pharmacist,
Lindo’s Pharmacy, Devonshire

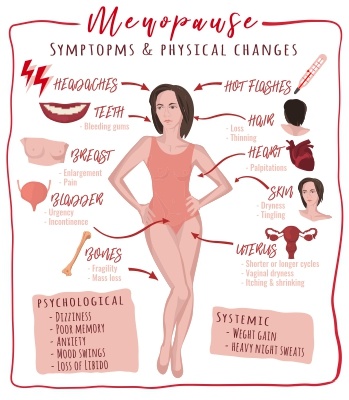
Women’s health differs from that of men in many unique ways.
Every March, we celebrate Women’s Month and the efforts, achievements, and force of womankind. However, amongst this applause is an equally important campaign for equality – a goal that unfortunately remains elusive in the US and worldwide. From pay to domestic labour, the imbalance between men and women is still rife throughout society – and healthcare is far from exempt.
A lack of research
So why are women facing inequality when it comes to their health? A key reason is research. Women’s health remains highly unresearched which, in turn, results in poorer health outcomes.
Throughout history, the majority of research and drug trials have been conducted on male participants on the (inaccurate) assumption that women are simply ‘smaller men’. Even when women have been included, they have only participated in tests during the early follicular phase of their menstrual cycle, when hormone levels are at their lowest and they are most like men.
As a result, critical drugs, treatments, and cures are not as effective on women – many have even been found to be harmful. Dosages can often be incorrect leading to adverse reactions, and inaccurate diagnoses are far more common. For example, women are 50 percent more likely to be misdiagnosed after a heart attack – unsurprising as they made up only a quarter of participants in core trials for congestive heart failure between 1987 and 2012.
 Gynaecological conditions
Gynaecological conditions
The Food and Drug Administration (FDA) in fact excluded females of ‘child-bearing potential’ from clinical trials from 1977 through 1993. The fear was that new treatments might harm their fertility, yet this has left a significant gap in the understanding of women’s fertility as well common gynaecological conditions that impact countless women’s lives.
Endometriosis, for example, is thought to impact approximately 11% of women worldwide. This condition causes severe pelvic pain especially during periods or after sex and can be debilitating for those who suffer from it. Despite its life-limiting symptoms, however, it can take up to 8 years for women to be diagnosed and treated.
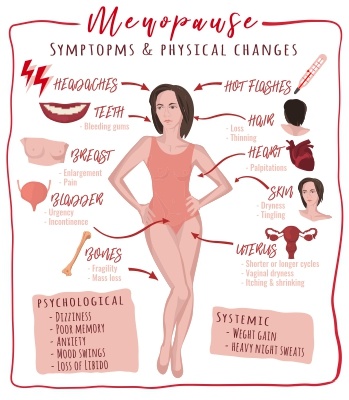
Similar issues like heavy menstrual bleeding, pregnancy complications, and menopause symptoms can often be overlooked too. Despite the debilitating – and sometimes fatal – impact menopause can have on women’s mental health, it is still difficult for women to access support and medications such as hormone replacement therapy (HRT), often due to a lack of understanding.
A wider impact
As we all know, when your health isn’t great, it can impact widespread areas of your life. With reduced access to effective healthcare, women are therefore placed at a disadvantage in the wider world.
Take the workplace, for example. With less effective treatment, women with health struggles are less able to participate and progress in the working world. This is particularly evident in the large numbers of older women reducing hours or resigning from leadership roles due to insufficient treatment for menopause, thus reducing female representation at senior levels.
What can be done?
The good news? Things are changing. Thanks to campaigns like International Women’s Day, awareness of this disparity is growing, prompting new studies, procedures, and treatments to help address the imbalance and improve women’s access to effective health care.
In the meantime, your pharmacist is here to help. Pregnant? We can provide vital support, advice, and a wide range of helpful products like supplements (try Pregnacare or Materna) to keep your iron levels up) and stretch mark creams like Bio-Oil or Palmer’s Stretch Mark cream. Going through the menopause? We can advise on therapies like HRT and offer cooling products like Estroven, Evening Primrose Oil or Culturelle to help with digestive issues that can arise during this time.
Whatever your gender, we will provide support and advice to help you feel your best. We will do our best to rectify any health inequalities and promote better health care for women in the years to come.
If you are concerned about your health, please contact your GP as soon as possible.
Stephanie Simons is the head pharmacist at Lindo’s Pharmacy in Devonshire. She earned her Bachelor of Science in Pharmacy at Massachusetts College of Pharmacy and has been practicing for over 20 years. She is a registered pharmacist with the Bermuda Pharmacy Council and is a member of the Bermuda Pharmaceutical Association.

 You can ease the symptoms by using products containing sodium citrate or potassium citrate such as Cymalon or Care Cystitis Relief which reduce the acidity of your urine to help prevent burning or irritating sensations. Phenazopyridine can also help to reduce pain and the sense of urgency to urinate. You may also need antibiotics to combat the infection; speak to your pharmacist or GP for advice.
You can ease the symptoms by using products containing sodium citrate or potassium citrate such as Cymalon or Care Cystitis Relief which reduce the acidity of your urine to help prevent burning or irritating sensations. Phenazopyridine can also help to reduce pain and the sense of urgency to urinate. You may also need antibiotics to combat the infection; speak to your pharmacist or GP for advice.